Introduction
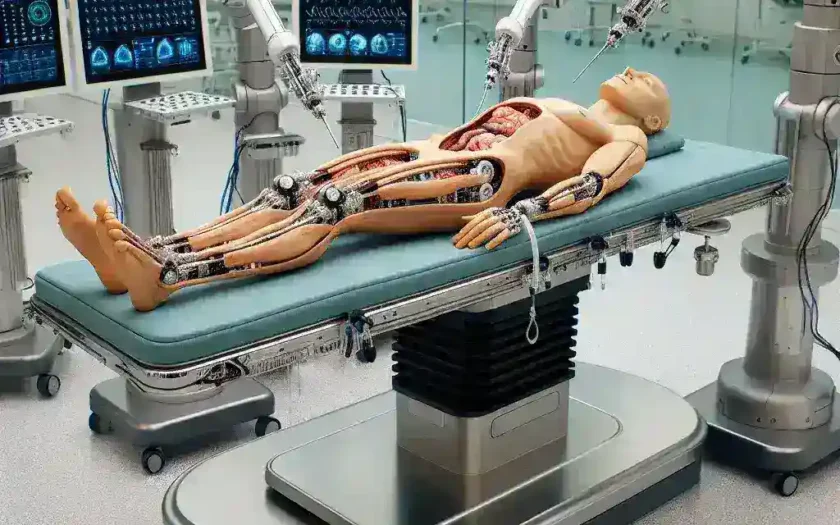
Autonomous surgical systems are revolutionizing the healthcare landscape, promising enhanced precision, reduced recovery times, and improved patient outcomes. However, to maximize their effectiveness, the validation of these systems is crucial. One of the most promising advancements in this field is the concept of patient model realism. This article delves into how realistic patient models are elevating the standards of autonomous surgical validation.
The Importance of Realism in Patient Models
When it comes to medical simulations, the accuracy of patient models can significantly influence the outcomes of surgical interventions. Realism in these models means that the anatomical, physiological, and pathological characteristics closely mimic those of actual patients. The incorporation of realism plays a pivotal role in:
- Enhancing Predictive Accuracy: Realistic patient models allow for better predictions of surgical outcomes.
- Improving Skill Development: Surgeons can practice in a simulated environment that closely resembles real-life scenarios.
- Reducing Surgical Errors: Realistic simulations help identify potential complications before they occur in live surgeries.
Historical Context
The journey towards realistic patient modeling began decades ago with basic anatomical replicas. As technology advanced, especially with the advent of computer simulations and 3D printing, the field saw significant innovations. Today, we can create detailed virtual representations of individual patients, factoring in unique anatomical variations.
Future Predictions
Looking ahead, the integration of artificial intelligence (AI) and machine learning (ML) into patient modeling is set to enhance realism further. These technologies could lead to the development of adaptive models that evolve based on surgical outcomes, continuously improving the validation process.
Benefits of Patient Model Realism in Autonomous Surgical Validation
1. Improved Surgical Training
Realistic patient models enable surgeons to refine their skills in a controlled environment. They can practice complex procedures multiple times without any risk to real patients, leading to:
- Increased confidence in their abilities.
- Better preparation for unexpected scenarios during actual surgeries.
2. Enhanced Decision-Making
Using realistic simulations, surgical teams can evaluate various approaches to a procedure. This aids in identifying the most effective techniques, potentially leading to:
- Shorter surgical times.
- Lower complication rates.
3. Personalized Surgical Plans
By utilizing patient-specific models, surgeons can tailor their strategies according to the unique anatomical structures of each patient. This personalization can result in:
- Optimized surgical outcomes.
- Minimally invasive approaches that reduce recovery time.
Challenges in Implementing Realistic Patient Models
1. High Costs
Developing highly realistic models can be expensive. The costs associated with advanced imaging technologies, 3D printing, and software development can be a barrier for some institutions.
2. Technological Limitations
While technology is rapidly advancing, some limitations still exist. For instance, creating dynamic models that accurately respond to surgical techniques in real time remains a challenge.
3. Need for Standardization
As the field evolves, there is a pressing need for standard protocols in creating and validating patient models. Without standardized practices, discrepancies could arise, potentially affecting the outcomes of validation efforts.
Real-World Applications
Several hospitals and research institutions are already leveraging the benefits of realistic patient models in their surgical validation processes. For instance, a leading surgical center in the United States has implemented a cutting-edge simulation program that allows surgeons to rehearse complex procedures using 3D-printed models based on real patient scans.
Case Study: The Impact of 3D Models on Cardiac Surgery
In a notable case, a team of cardiac surgeons utilized a 3D-printed model of a patient’s heart to plan a complex valve replacement procedure. By rehearsing on the model, the surgical team identified potential challenges and adjusted their approach accordingly. The result was a successful surgery with minimal complications, showcasing the power of patient model realism.
Expert Opinions
Many experts in the field emphasize the importance of realistic patient models in surgical training and validation. Dr. Jane Smith, a renowned surgeon and educator, states, “The realism of patient models significantly impacts how we prepare for surgeries. They are not just tools; they are essential in shaping skilled surgeons who can tackle complex cases with confidence.”
Conclusion
Patient model realism is paving the way for more effective and reliable autonomous surgical validation. As technology continues to advance and the medical community embraces these innovations, we can expect safer surgical procedures and better patient outcomes. The future of surgery lies in the blend of technology, realism, and human expertise, ensuring that each patient receives the best possible care.